Recovering from a complex spinal cord injury (SCI) is never one-size-fits-all. These injuries can range in severity and presentation from complete paralysis to partial sensory or motor loss. Each case requires a tailored, team-based plan.
In a expert-led webinar hosted by Medical and Life Care Consulting Services, Dr. Jerrold Kaplan of Gaylord Specialty Healthcare shared cutting-edge insights into the recovery process, advanced therapeutic tools, and what it takes to help patients return to work and life.
Here’s a breakdown of the critical insights from the session, including key rehabilitation stages, common challenges, and modern interventions that are changing the game.
Understanding the Injury: Types & Classifications
Spinal injuries are categorized using the ASIA Impairment Scale, ranging from A (complete injury) to E (normal function). Most injuries fall between C3–C5 in the cervical spine and can be classified as:
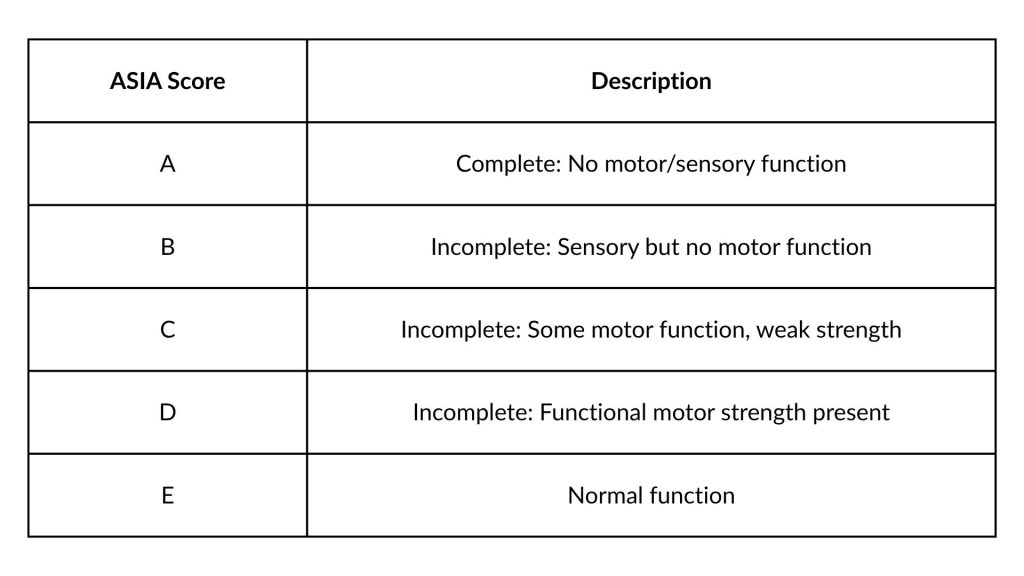
SIA Neurological Classification Tool
Standard ASIA chart used for evaluating motor and sensory function after spinal cord injury.
This form helps clinicians map motor control (e.g., elbow flexors at C5, hip flexors at L2) and sensory response to classify injury levels and guide rehab planning.
The Power of Interdisciplinary Rehab
One of the most significant takeaways? Recovery success hinges on early and coordinated interdisciplinary care.
Core Team Members:
- • Physiatrist (Physical Medicine & Rehab Physician)
- • Physical & Occupational Therapists
- • Respiratory Therapists
- • Psychologists
- • Social Workers
- • Case Managers
Unlike a multidisciplinary model, the interdisciplinary approach ensures that all professionals communicate consistently and plan collaboratively—leading to better patient outcomes
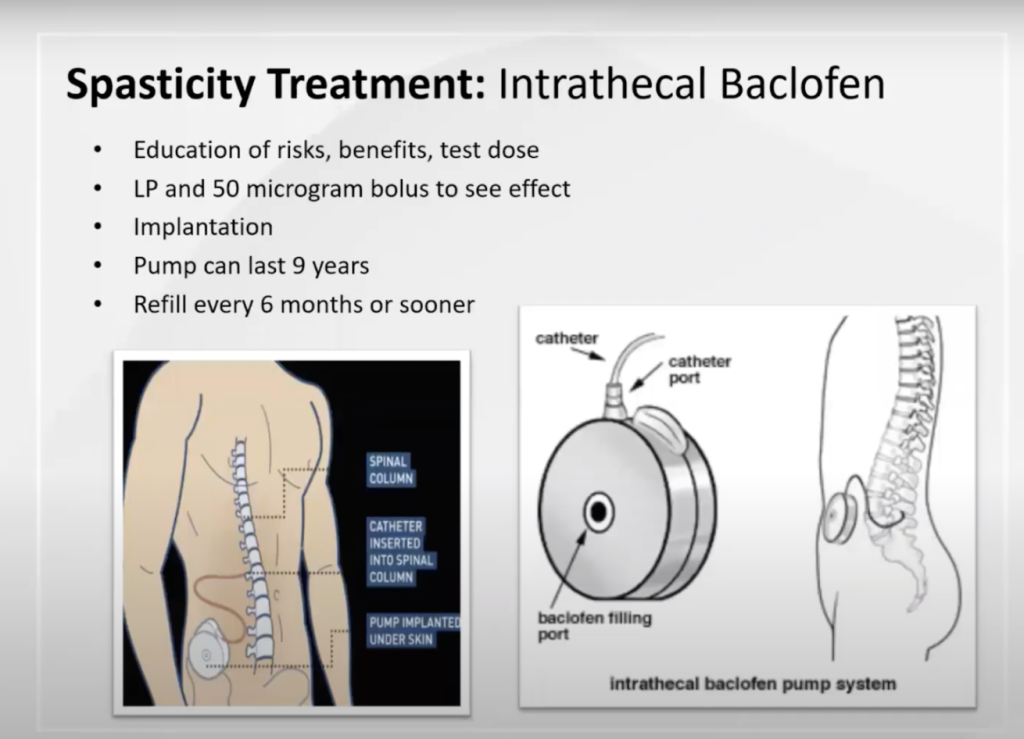
Intrathecal Baclofen Pump System
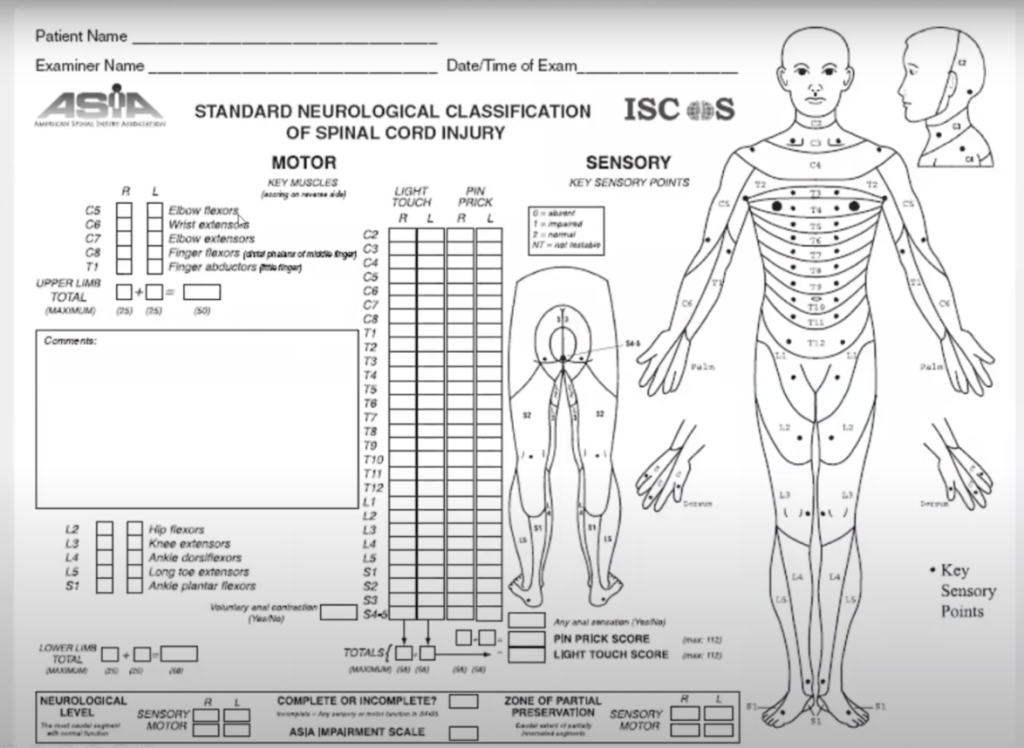
Diagram of an implanted intrathecal baclofen pump delivering medication directly to the spinal cord.
Key Notes:
- • Pump implanted under the skin
- • Connected to spinal cord via catheter
- • Lasts up to nine years
- • Refills every six months (or sooner)
This is a critical option for improving function in individuals with severe spasticity who haven’t responded to traditional treatment.
Key Components of Spinal Cord Injury Rehab
1. Levels of Care (Post-Acute Options):
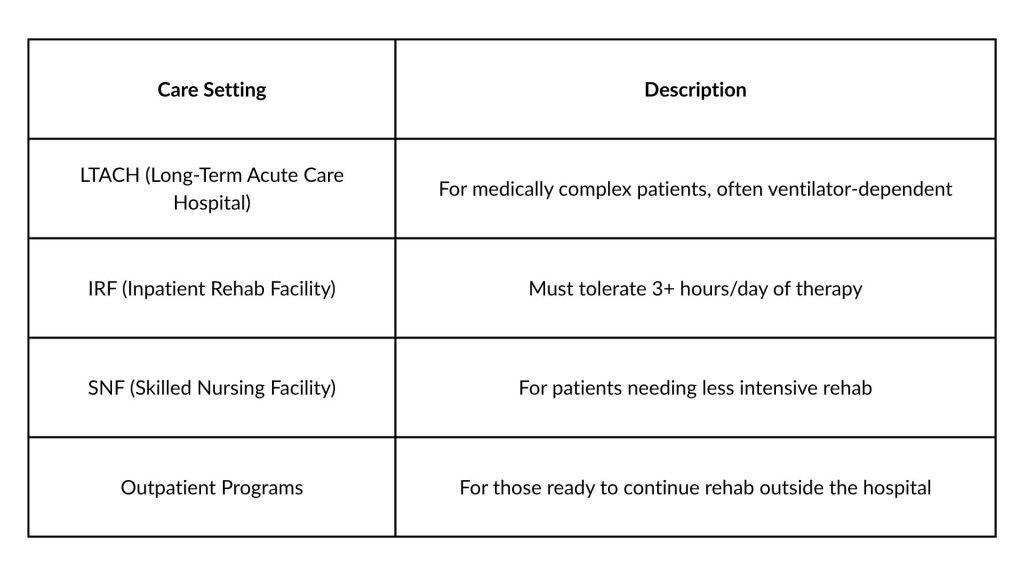
Each level has different therapy intensities and admission requirements. Choosing the right path is vital for functional gains.
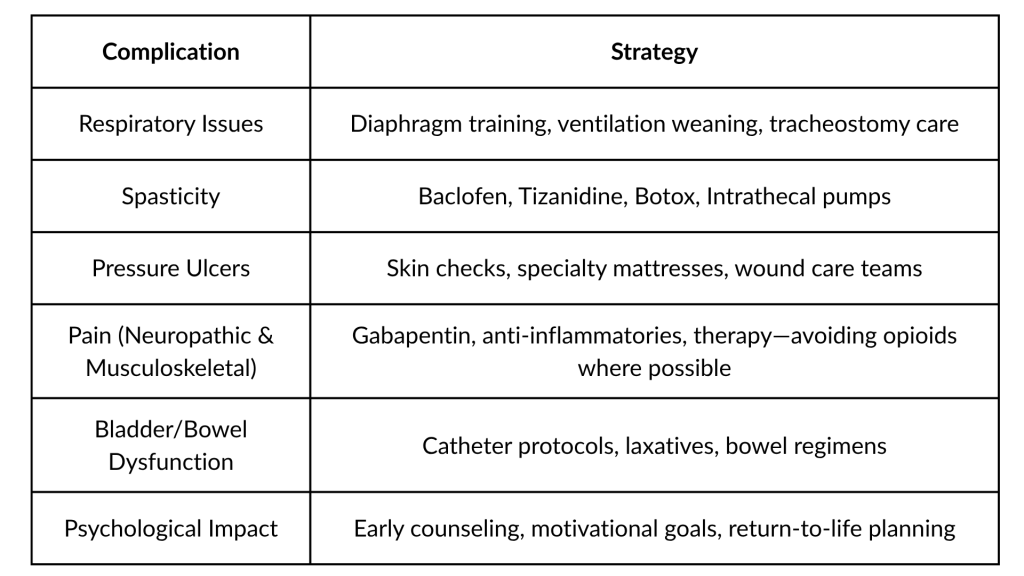
2. Common Challenges & Management
3. Advanced Tech & Therapies for Recovery
Modern recovery tools are changing what’s possible for SCI patients:
- • Functional Electrical Stimulation (FES): Stimulates muscle activity and circulation.
- • Zero-G & Alter-G: Body-weight-supported treadmills for safe gait training.
- • EXO & ReWalk Devices: Robotic exoskeletons enabling mobility in complete SCI cases.
- • KinserQ & Bioness Systems: Visual-motor training and balance retraining.
- • Adaptive Sports & Aquatic Therapy: Build confidence, strength, and social reintegration.
4. Return to Work: Conditioning & Hardening
Helping individuals get back to work—especially in physically demanding roles—requires more than just physical therapy:
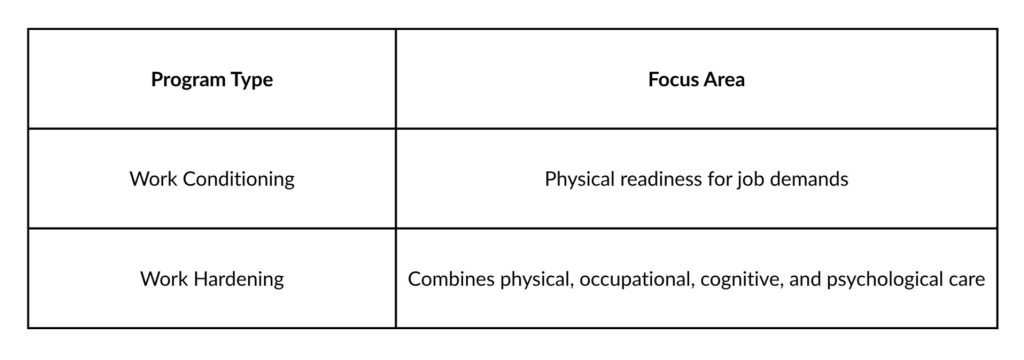
A firefighter may need to train with a 70-pound suit; a dispatcher may need assistive technology. These programs recreate real-world scenarios to restore confidence and competence.
Final Thoughts: Start Early, Stay Consistent
One of the most consistent themes throughout the webinar was avoiding delays in rehabilitation. Early intervention prevents secondary complications and maximizes functional gains. Likewise, consistent outpatient care without insurance delays or therapy gaps—is crucial for momentum and morale.
“If we tell patients early on that they will never walk again, it becomes a self-fulfilling prophecy. Empowering them with possibility makes all the difference.”
Dr. Jerrold Kaplan
Want to learn more about post-injury planning or consult with specialists in medical case management?
Explore Medical and Life Care Consulting Services for tailored recovery solutions.