In the fourth and final session of the Injury Insight series, Dr. Charles Cassidy—Chairman of Orthopedics at Tufts University—shared invaluable perspectives on the diagnosis, treatment, and recovery of common upper extremity injuries. Hosted by Medical and Life Care Consulting Services, the session aimed to educate case managers, HR professionals, and clinicians on injuries that often challenge recovery processes and claim management.
Here are the core takeaways:
The Hand-Brain Connection: Why Upper Extremity Injuries Matter
One standout concept emphasized by Dr. Cassidy was the neurological significance of hand injuries. As represented in the homunculus map, a disproportionately large area of the brain is dedicated to hand function. This explains why hand injuries can feel devastating—even traumatic—causing psychological stress and perceived permanent disability.
Common Psychological Barrier: Catastrophization
Dr. Cassidy highlighted catastrophization as a major recovery inhibitor, where patients believe their condition will never improve. Signs include:
• Avoidance of using the injured hand
• Unusual hand posture or protective behavior
Early intervention and patient education are crucial.
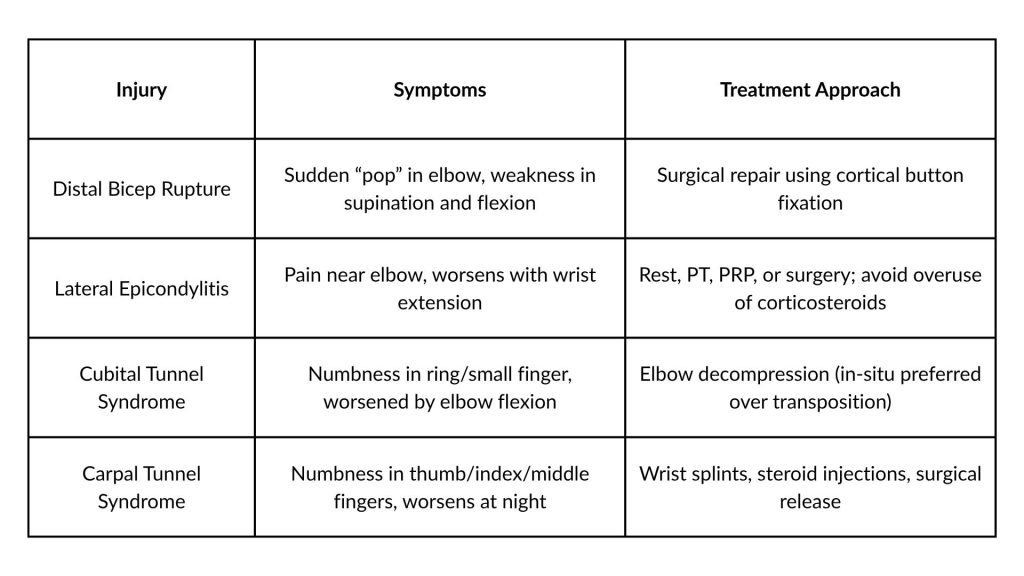
Key Injuries & Treatment Insights
The Steroid Injection Debate: Myths & Facts
Dr. Cassidy addressed common myths around steroid injections:
• Rupture Risk: Extremely low when injected correctly.
• Accelerated Arthritis: Possible with repeated joint injections in younger patients.
• Hyperglycemia: A concern mainly for insulin-dependent diabetics.
• Fat Atrophy & Depigmentation: Common with certain steroid types—use water-soluble forms for safety.
PRP vs Steroid: Which One Wins?
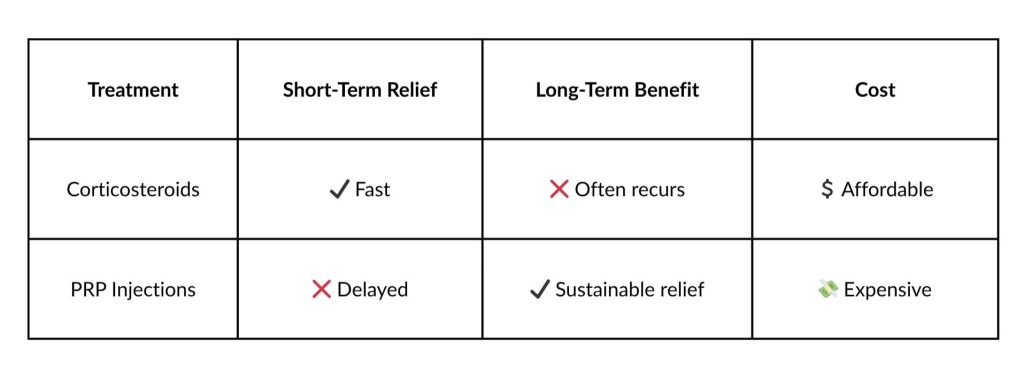
Note: Most experts, including Dr. Cassidy, recommend no more than three PRP injections before considering surgery.
Diagnostic Tools: When & What to Use
• EMG/Nerve Studies: Ideal for cubital and carpal tunnel syndrome, especially when surgery is considered.
• MRI/X-ray: Reserved for unusual presentations or trauma.
• Hand Pain Diagrams: A surprisingly effective and simple diagnostic aid.
Conservative vs Surgical Management: Decision Factors
When to consider surgery:
• Conservative treatments have failed for 6+ months
• Significant strength loss or nerve dysfunction
• Persistent symptoms impacting work and daily activities
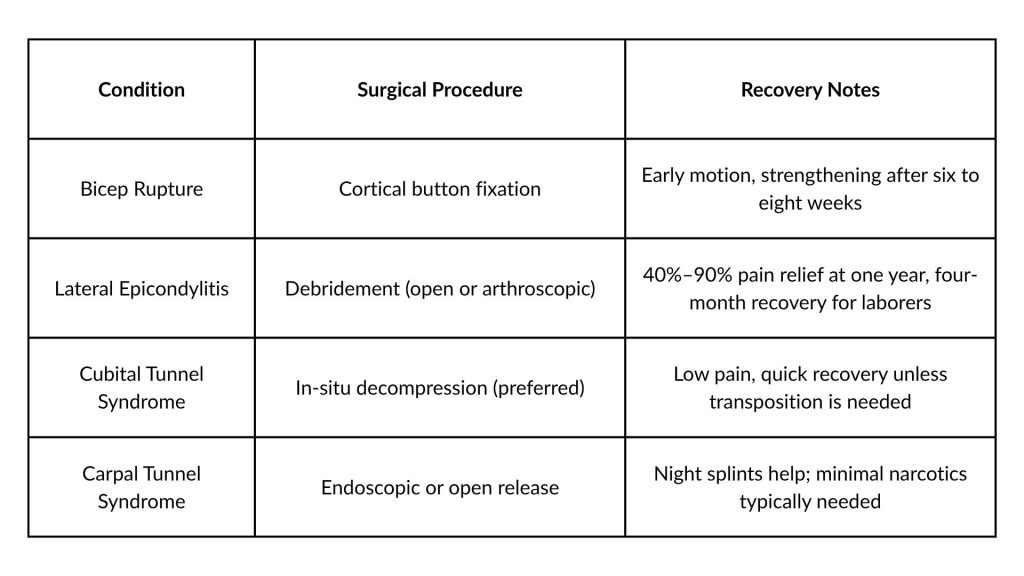
Surgical Options Overview:
Final Thoughts: Empower Patients Through Education
Dr. Cassidy stressed that education is key. Most post-op discomfort is manageable with:
• Early mobilization
• Alternating NSAIDs and acetaminophen
• Setting realistic expectations
Conclusion:
Upper extremity injuries, though common, are often misunderstood and mismanaged. Armed with expert insights from Dr. Cassidy, clinicians and case managers can better guide patients through diagnosis, treatment, and full recovery.






